Generally, Alzheimer’s diagnosis comes too late in the game. This may change, because now researchers have developed a DNA-based approach to identifying people who have an increased genetic risk to the disease.
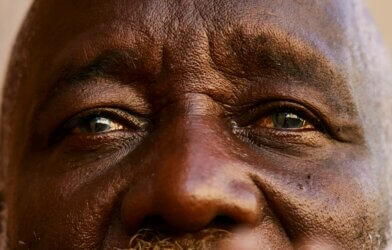
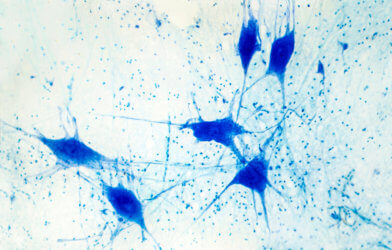
People with Alzheimer’s disease usually experience neurodegeneration gradually, which is one of the reasons that it’s so difficult to catch at the right time. Though there are treatments out there that can relieve a patient of some of the harsh symptoms, disease progression continues to happen at a steady pace and usually can’t be stopped.
Previously, clinical trials have investigated treatments, but testing on patients who have late-stage Alzheimer’s make it much harder to find success. It’s been a race against the click to identify more effective screening and treatment, improving outcomes for those at-risk and who currently have it.
To aid this effort, Manish Paranjpe, from the Broad Institute of MIT and Harvard University, and colleagues analyzed DNA variants across 7.1 million people. Participants’ data came from an earlier study that included thousands of healthy individuals and ones with Alzheimer’s disease. With this data, they developed a method that determines someone’s risk for the disease depending on the type of DNA variant that someone possesses. They took this information and further touched up their work, and added 300,000 more people to the set.
“We developed a genetic predictor of Alzheimer’s disease associated with both clinical diagnosis and age-dependent cognitive decline. By studying the circulating proteome of healthy individuals with very high versus low inherited risk, our team nominated new biomarkers of neurocognitive disease,” says senior author Dr. Amit V. Khera in a statement.
To see if there is promise in clinical settings, they applied the method by conducting disease risk prediction in 636 blood donors, scouring their blood for any of the thousands of proteins that can flag them as high-risk. They discovered 28 proteins that could be associated to Alzheimer’s risk, several with no research at all within this field of study. By taking a deeper look through experimentation with these proteins, scientists could unravel new paths toward improved cared and treatment.
The team has noted that as of now, this method is not easily applicable for most physicians as it’s not been well-tested in diverse populations. They also note that a clear limitation is how insurance will be able to cover the tests required, presenting a challenge especially for those who are low-income. However, they believe in working out the kinks for more efficient Alzheimer’s care processes.
This study is published in the journal PLoS Genetics.