The placebo effect refers to a patient’s symptoms improving because the patient expects a treatment to be effective, but not from specific effects of the treatment itself. But how exactly does this happen? Researchers from Massachusetts General Hospital (MGH) and Sunnybrook Health Sciences Center, University of Toronto, have, for the first time, discovered indications of a neurological mechanism for the placebo effect.
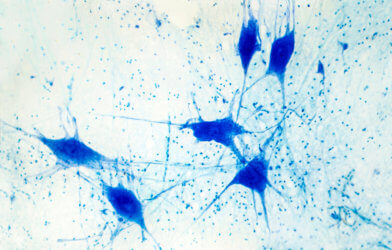
Imaging studies identify a pattern of changes in certain brain regions when a person experiences this phenomenon. The findings enhance understanding of placebo effects, and could influence interpretation of clinical trials of brain stimulation. Their work may lend insight about harnessing placebo effects for treatment of a variety of conditions.
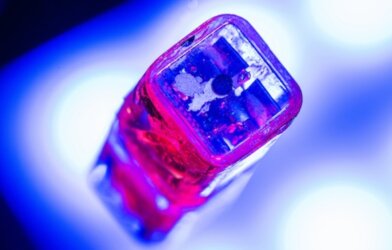
Transcranial magnetic stimulation (TMS) is a non-invasive treatment for depression that doesn’t respond adequately to medication or psychotherapy. It has been gaining wider use in recent years. A coil is applied to the patient’s head, which delivers electromagnetic pulses to the brain. The TMS effect on brain activity has been established during the last 30 years. Several TMS devices are approved by the Food and Drug Administration for treating depression.
Emiliano Santarnecchi, PhD, director of Precision Neuroscience & Neuromodulation at MGH’s Gordon Center for Medical Imaging, saw studies of brain stimulation as a unique opportunity to learn more about the neurobiology of the placebo effect and deep brain stimulation (DBS.)
Santarnecchi and his team conducted a meta-analysis and review of neuroimaging studies involving both healthy subjects and patients. They were able to create a map of brain regions activated by the placebo effect. They also analyzed studies of people treated with TMS and DBS for depression to identify brain regions targeted by the therapies. The team found sites in the brain activated by the placebo effect overlapping with brain regions affected by TMS and DBS.
Santarnecchi and his colleagues discovered that the overlap is critical to interpreting the results of research on brain stimulation for conditions such as depression. In a clinical setting, depression patients receiving brain stimulation improve—but so do many patients receiving placebo treatment. That led to confusion about the benefits of therapy. A possible explanation is “that there is a significant placebo effect when you do any form of brain stimulation intervention,” speculates Santarnecchi.
Unlike taking a pill, TMS is administered in a surgery-like setting, with imaging monitors and a clinician applying a coil to the patient’s head. Each pulse makes a loud click. “So, the patient thinks, ‘Wow, they are really activating my brain’, so you get a lot of expectation,” says Santarnecchi.
According to neurologist Dr. Matthew Burke, of Sunnybrook Health Sciences Center in Toronto, greater placebo effects associated with brain stimulation makes it difficult to study. If brain stimulation and the placebo effect activate the same brain regions, those circuits could be maximally activated by placebo effects, which could make it difficult to show any additional benefit from TMS or DBS. Separating the placebo component of brain stimulation interventions from the TMS or DBS direct impact on brain activity will help to design studies in which techniques such as TMS will be more reliably quantified. Accurate information will improve the efficacy of treatment protocols.
Santarnecchi says, “We think this is an important starting point for understanding the placebo effect in general, and learning how to modulate and harness it, including using it as a potential therapeutic tool by intentionally activating brain regions of the placebo network to elicit positive effects on symptoms.”
The study authors are designing trials that will separate the effects of brain stimulation from placebo effects and offer insights about leveraging the placebo effect in clinical settings. Their paper is published in Molecular Psychiatry.