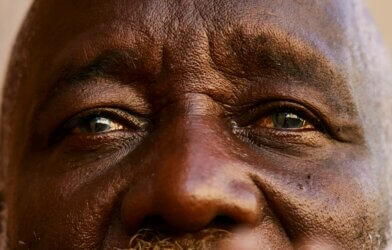
Psychedelic drugs are commonly considered to be “rave” or recreational drugs that can take the mind to another place. Not as widely known yet is that they also have been studied and used on people with anxiety, chronic headaches, depression, and other mood disorders. These drugs have shown great benefits in serotonin receptors the past, specifically with mood regulation, appetite, cognition and emotion. Not everyone responds the same way to all drugs, though. Why are some individuals experiencing greater mental health benefits than others?
Researchers from the University of North Carolina at Chapel Hill set out to address this. In a recent paper, they report that the body’s responses to a particular psychedelic drug may be due to genetic variations in a specific serotonin receptor.
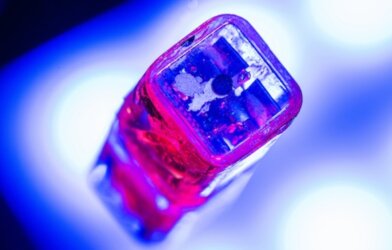
With a restored interest among neurology researchers in the use of psychedelics for treatment, this study has been fully embraced by the field. To conduct the work, Dr. Bryan Roth and his team utilized several assays to measure the effect that seven different single nucleotide polymorphisms (SNPs), the most common type of genetic variation, had on in-vitro binding and signaling of the 5-HT2A serotonin receptor when exposed to four different psychedelics.
The study involves four different psychedelic drugs, because this methodology would allow specific examination of structure and function of the receptor of interest. Additionally, SNPs are exceedingly common, and often random. They chose psilocybin, LSD, 5-MeO-DMT (found in toad venom), and mescaline.
The results show that some variations, even ones far from the binding site, altered the way the serotonin receptor interacted with the drugs. Based on these findings, the team expects that people with contrasting types of variations would react differently to psychedelic drug treatments. This essentially means that there could be a completely different response to a certain drug across different patients depending on genetic makeup that affects expression of serotonin receptors.
For instance, an SNP called Ala230Th showed increased and decreased reactions to each of the drugs tested, whereas the original form of the gene did not. On the other hand, a mutation of the His452Th gene only reacted less, showing no increase at all.
Study authors propose that physicians and other healthcare providers take serotonin-related genetics more seriously in patients with mental health conditions. Not only can this improve identification measures used to determine which psychedelic is most appropriate, but also other types of medications commonly used for these disorders. Traditional treatments don’t always work for patients, but scientists don’t always exactly know why. This team believes the answer may lie in the genes.
This study is published the journal ACS Chemical Neuroscience.