Alzheimer’s disease is a devastating condition that causes progressive memory loss, cognitive decline, and disability in old age. It affects millions of people worldwide, but current treatments can only modestly slow symptom progression at best. However, a new study from researchers in the United Kingdom has identified a promising therapeutic target that could help prevent some of the damaging effects of Alzheimer’s.
The target is an enzyme called phosphodiesterase-4B (PDE4B). Previous large-scale genetic studies had suggested that PDE4B might play a role in Alzheimer’s, but its exact involvement wasn’t clear. To investigate further, researchers utilized a special laboratory mouse model of Alzheimer’s disease called the App knock-in mouse for the study published in the journal Neuropsychopharmacology.
What makes the App knock-in mouse a good model is that it develops many key features of human Alzheimer’s disease as it ages, including accumulation of toxic amyloid-beta protein, inflammation in the brain, synapse damage, and memory deficits. Unlike some other mouse models, though, App knock-in mice have more physiologically realistic levels of amyloid precursor protein, making it a highly authentic model.
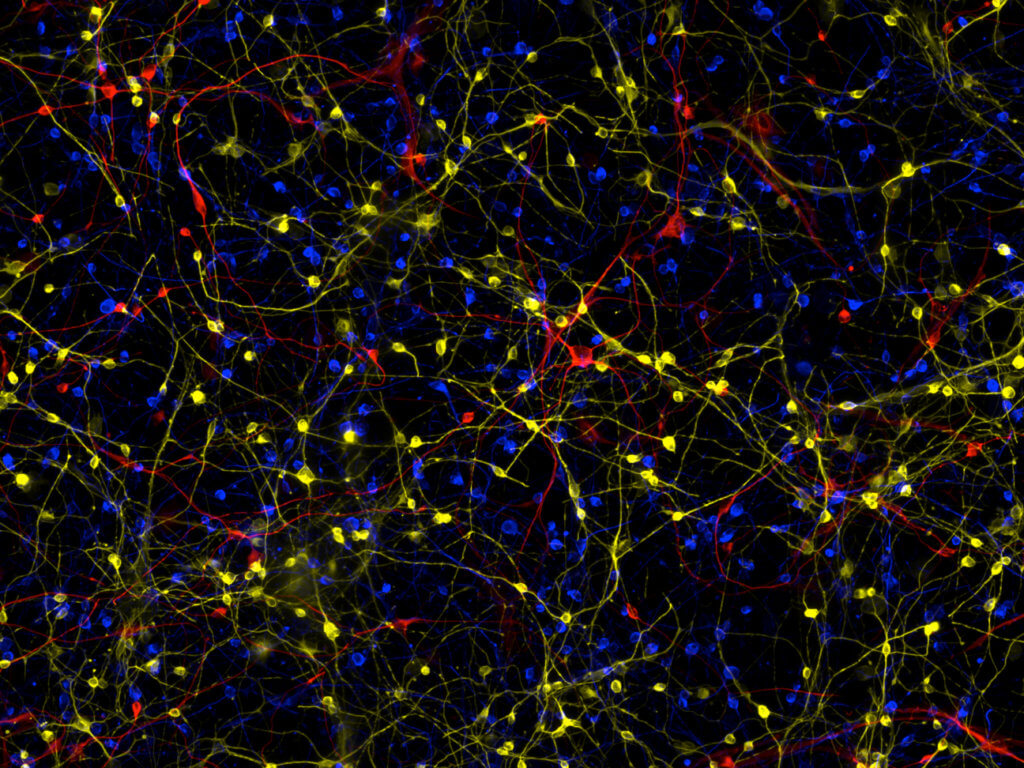
Researchers took App knock-in mice and bred them with mice that had a mutation causing reduced PDE4B enzyme activity. PDE4B normally breaks down an important signaling molecule in cells called cyclic AMP (cAMP). By partially “inhibiting” PDE4B, the mutation allows cAMP levels to stay a bit higher.
At 1 year old, an age when App knock-in mice normally show significant memory problems, the researchers tested the mice’s spatial memory using a special circular maze filled with holes called the Barnes maze. Normal App mice took much longer to learn and remember how to find the target hole compared to healthy mice. Remarkably though, App mice with the PDE4B mutation performed just as well as healthy mice, showing that reduced PDE4B activity protected their spatial memory.
Scientists then measured the brain activity of the mice using a sophisticated technique called 14C-2-deoxyglucose autoradiography. This allowed them to map glucose energy metabolism in the brain, which is reduced in many regions in Alzheimer’s. Sure enough, while App mice had lower brain metabolism compared to healthy mice, the App mice with reduced PDE4B had normalized brain metabolism, matching the healthy mice.
When the researchers looked at levels of amyloid-beta plaques in the brains of the mice, they found no differences between App mice with normal or reduced PDE4B. This suggests that the cognitive benefits of PDE4B inhibition weren’t due to lowering amyloid, but rather through other mechanisms. Researchers did find that reduced PDE4B helped dampen levels of certain inflammatory molecules in the brain that were elevated in the App mice.
“Reducing the activity of the PDE4B enzyme had a profound protective effect on memory and glucose metabolism in the AD mouse model, despite these mice showing no decrease in the number of amyloid plaques in the brain,” says study lead author Dr. Steven Clapcote, from the University of Leeds, in a media release. “This raises the prospect that reducing PDE4B activity may protect against cognitive impairment not only in Alzheimer’s disease but also in other forms of dementia, such as Huntington’s disease.”
Finally, scientists compared the activation levels of different genes in the brains of normal mice, App mice, and App mice with reduced PDE4B. They found a number of genes whose activity seemed to be normalized by inhibiting PDE4B, identifying them as potential molecular mediators of PDE4B’s protective effects. Notable among these were genes involved in inflammation and the gene for insulin-degrading enzyme, which helps break down amyloid-beta.
“These results offer real hope for the development of new treatments that will benefit patients with Alzheimer’s disease in the future,” explains study co-author Dr. Neil Dawson, from Lancaster University. “It was intriguing to find that reducing PDE4B activity by just 27 percent could dramatically rescue memory, brain function and inflammation in the AD mice. The next stage is to test whether PDE4B inhibiting drugs have similar beneficial effects in the AD mouse model, to test their potential efficacy in Alzheimer’s disease.”
While much more research is still needed, the results raise the exciting possibility that drugs targeting PDE4B could provide a new way to combat the progression of Alzheimer’s by normalizing brain function and inflammation, rather than directly attacking amyloid plaques. The findings also underscore the importance of understanding the complex molecular changes Alzheimer’s causes in the brain, beyond just amyloid-beta itself.