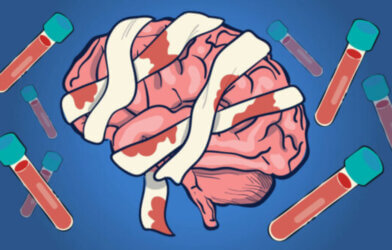
A pioneering new study has revealed a simple blood test that could dramatically improve outcomes for stroke patients. By detecting a specific type of stroke caused by large vessel blockages, this test could ensure patients receive life-saving treatment as quickly as possible.
The study, published in the journal Stroke: Vascular and Interventional Neurology and led by researchers at Brandon Regional Hospital in Florida and Harvard Medical School, followed over 300 suspected stroke patients who arrived at the hospital within 18 hours of their symptoms starting. Researchers took blood samples and measured levels of two key proteins — GFAP and D-dimer.
GFAP, or glial fibrillary acidic protein, is a protein released by brain cells when they are damaged, such as during a stroke. Prior research has shown that GFAP levels tend to be particularly high in brain bleeds or hemorrhagic strokes. D-dimer, on the other hand, is a small protein fragment present in the blood after a blood clot is degraded by the body’s own enzymes. D-dimer levels tend to be elevated in blood clot-related or ischemic strokes.
Researchers found that by using specific cut-off levels for GFAP and D-dimer (213 pg/mL and 600 ng/mL respectively) and combining these biomarker results with existing clinical stroke severity scales like FAST-ED, they could identify patients suffering from a severe form of ischemic stroke known as a “large vessel occlusion” or LVO with a high degree of accuracy.
“We have developed a game-changing, accessible tool that could help ensure that more people suffering from stroke are in the right place at the right time to receive critical, life-restoring care,” says senior study author Dr. Joshua Bernstock, a clinical fellow in the Department of Neurosurgery at Brigham and Women’s Hospital.
LVOs occur when one of the brain’s major arteries becomes blocked by a clot, cutting off blood supply to a large portion of the brain. They are responsible for the most severe, debilitating strokes and require swift treatment with a procedure called thrombectomy to surgically remove the clot. However, thrombectomy is only available at specialized stroke centers, so rapidly identifying LVO patients and getting them to the right hospital is critical.
“Mechanical thrombectomy has allowed people that otherwise would have died or become significantly disabled be completely restored, as if their stroke never happened,” explains Dr. Bernstock. “The earlier this intervention is enacted, the better the patient’s outcome is going to be. This exciting new technology has the potential to allow more people globally to get this treatment faster.”
When researchers applied their GFAP/D-dimer test and clinical scale algorithm to suspected stroke patients arriving within 6 hours of symptom onset — the window when treatment is most effective — it correctly identified LVO strokes with an impressive 81 percent sensitivity and 93 percent specificity. In other words, it “caught” 81 percent of LVO cases while only misidentifying 7 percent of non-LVO strokes.
This high performance was achieved without misclassifying any of the dangerous brain hemorrhage cases that can resemble LVOs. The test accurately “ruled out” 100 percent of hemorrhagic strokes based on their high GFAP but low D-dimer levels. This is crucial because the clot-busting drugs and surgeries used for ischemic stroke could be fatal if given to a hemorrhage patient by mistake.
By comparison, the commonly used stroke severity scales on their own only had specificities in the range of 48-65 percent for detecting LVOs, leading to many “false alarms.” The addition of the GFAP/D-dimer blood test dramatically boosted their accuracy, especially in terms of not missing true LVOs while still weeding out the false positives.
Researchers emphasize that the true power of this test lies in its potential for use in ambulances and emergency rooms. By drawing blood immediately and plugging the GFAP and D-dimer values into the clinical scale algorithms, first responders could quickly identify probable LVO patients and rush them straight to the more distant specialty centers for thrombectomy, bypassing closer hospitals not equipped to treat them. The time saved could mean the difference between disability and recovery.
“In stroke care, time is brain,” concludes Dr. Bernstock. “The sooner a patient is put on the right care pathway, the better they are going to do. Whether that means ruling out bleeds or ruling in something that needs an intervention, being able to do this in a prehospital setting with the technology that we built is going to be truly transformative.”