A new study from the Leonard Davis School of Gerontology at the University of Southern California questions the current belief that buildup of a protein called amyloid beta (Aβ) is associated with neurodegeneration in Alzheimer’s disease. Is it possible that the protein relates to normal brain aging?
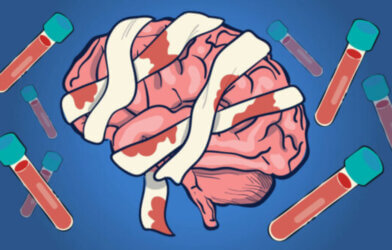
Professor in the neurobiology of aging, Caleb Finch, explored the levels of Aβ in human brains by analyzing tissue samples from both healthy brains and brains of patients with dementia. The analysis showed that older, but still cognitively healthy brains showed similar amounts of dissolvable, non-fibrillar amyloid protein as the brains of patients with Alzheimer’s disease. The brains of Alzheimer’s patients, however, had greater amounts of insoluble Aβ fibrils, the form of amyloid protein that forms the plaques seen in the disease, according to Max Thorwald, postdoctoral researcher.
The findings differ from the idea that just having greater amounts of amyloid protein is an underlying cause of Alzheimer’s, report Finch and Thorwald, in a statement. They speculate that the increase in soluble Aβ may be age-related, but not specific to Alzheimer’s. The higher levels of fibrillary amyloid seem to be a better indicator of disease. According to Thorwald, the problem may be a reduced ability to clear the protein, allowing formation of fibrillary amyloid, contributing to plaques.
“These findings further support the use of aggregated, or fibrillary, amyloid as a biomarker for Alzheimer’s treatments,” Thorwald said. “The site in which amyloid processing occurs has less precursor and enzyme available for processing, which may suggest the removal of amyloid as a key issue during Alzheimer’s.”
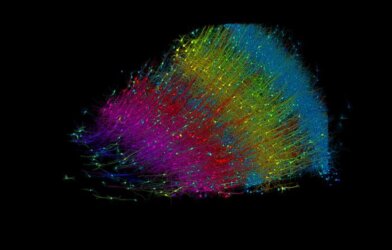
During early adulthood, amyloid levels increase, differing by brain regions. “The frontal cortex produces more amyloid than the cerebellum, consistent with their Alzheimer’s-associated pathologies in late life,” Thorwald said. “Future projects should examine amyloid over the life course in both cognitively normal and Alzheimer’s patients with both modulation of amyloid processing and removal of amyloid through monoclonal antibodies currently used in clinical trials for Alzheimer’s treatment.”
Lemanecab, a monoclonal antibody treatment, reduces Aβ plaques in clinical trials. It recently received FDA approval for its ability to slow cognitive decline in Alzheimer’s disease. Further research is needed, however, on its long-term impact. Finch said.
“Lecanemab clearly works to diminish fibrillar amyloid,” Finch said. “We are concerned with major side effects, however, including brain swelling and bleeding, that were 100% more than in controls, with unknown delayed or latent impact.”
Finch noted that very few cases of dementia occur with amyloid plaques, or masses of aggregated Aβ protein, as the only aberrance in affected brains. Most cases have complex tissue abnormalities, such as buildup of additional types of protein or small bleeds in the brain.
This information is published in Alzheimer’s and Dementia.