Powerful new treatments for neurological disorders could soon be on the horizon — all thanks to an innovative brain stimulation technique. Scientists from Mass General Brigham have mapped a “human dysfunctome” — a term describing a network of dysfunctional brain circuits linked to various conditions. This research, published in the journal Nature Neuroscience, uses deep brain stimulation (DBS) to precisely identify and target brain circuits that could potentially revolutionize the treatment for Parkinson’s disease, dystonia, obsessive-compulsive disorder (OCD), and Tourette’s syndrome.
DBS is a sophisticated medical procedure where electrical impulses are sent to specific parts of the brain to regulate abnormal impulses. The procedure, which involves implanting electrodes within certain areas of the brain, is used to treat a variety of neurological conditions.

“We were able to use brain stimulation to precisely identify and target circuits for the optimal treatment of four different disorders,” says study co-corresponding author Dr. Andreas Horn, from the Center for Brain Circuit Therapeutics in the Department of Neurology at Brigham and Women’s Hospital and the Center for Neurotechnology and Neurorecovery at Massachusetts General Hospital, in a media release. “In simplified terms, when brain circuits become dysfunctional, they may act as brakes for the specific brain functions that the circuit usually carries out. Applying DBS may release the brake and may in part restore functionality.”
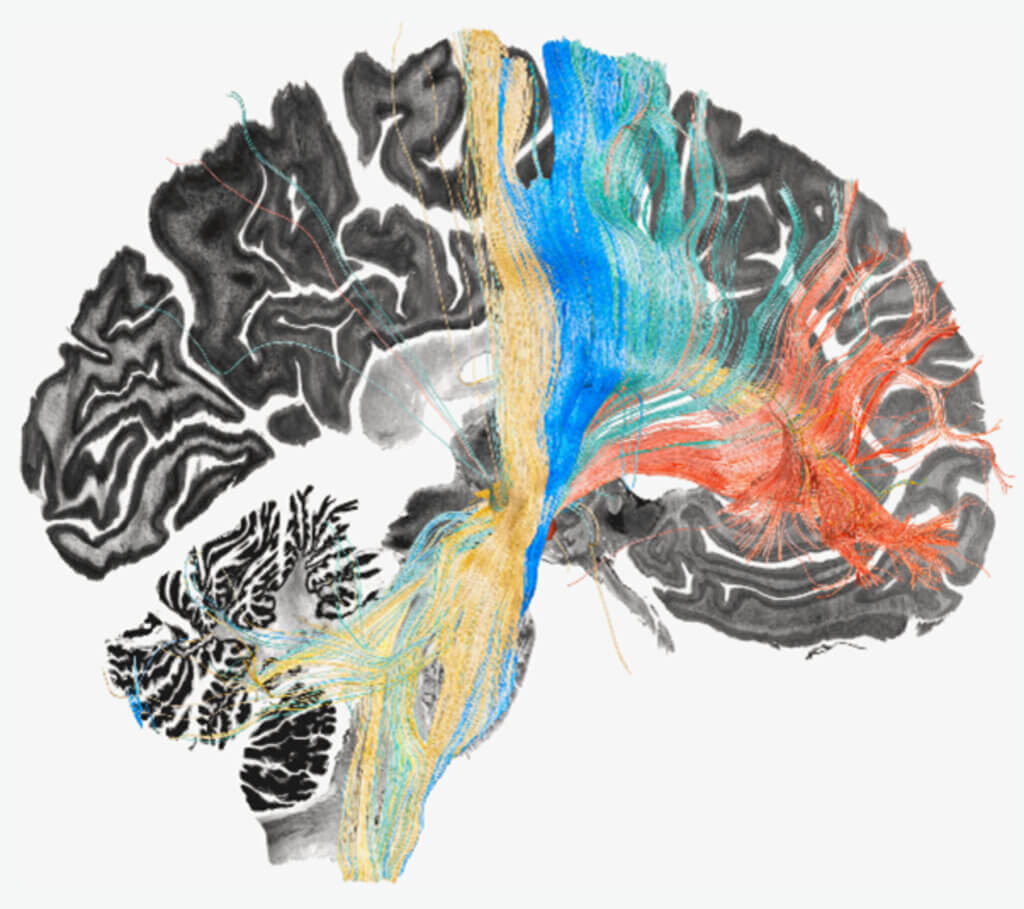
The study’s approach focuses on the connections between the frontal cortex, a part of the brain responsible for higher cognitive processes, and the basal ganglia, deep-brain structures involved in controlling movement and behavior. Dysfunctions in these connections can lead to the aforementioned neurological disorders. Previously, stimulating the subthalamic nucleus (a component of the basal ganglia that has extensive connections with the frontal cortex) has been shown to alleviate symptoms of these disorders, but the new study goes further by pinpointing specific dysfunctional circuits within these broader networks.
By analyzing data from 534 DBS electrodes implanted in 261 patients worldwide, researchers were able to map out the affected brain circuits with unprecedented precision. This mapping revealed that certain brain circuits, such as those in the sensorimotor cortices for dystonia, the primary motor cortex for Tourette’s, the supplementary motor area for Parkinson’s disease, and parts of the cingulate cortex for OCD, were particularly impacted. These findings suggest that interconnected pathways across different disorders may be disrupted, offering a new angle for treatment strategies.
The study not only sheds light on the underlying brain circuit dysfunctions in these disorders but also demonstrates the potential for refining DBS treatments to achieve better outcomes. One notable success story from the study involves a young woman in her early 20s with severe, treatment-resistant OCD. After receiving targeted DBS treatment, she showed significant improvement in her symptoms, including obsessions about food and water intake and compulsive skin picking, just one month after the procedure.
While the study primarily relied on retrospective data analysis, the promising results pave the way for further research.
“We can take this technique further and finely segregate dysfunctional circuits in order to have greater impact with treatment,” explains study lead author Barbara Hollunder, of the Movement Disorders and Neuromodulation Unit in the Department of Neurology at Charité–University Medicine Berlin. “For example, with OCD, we can look at isolating circuits for obsessions versus compulsions and so on.”
This research marks a significant advancement in understanding and treating neurological disorders, offering hope for more effective and personalized therapies in the future.