In the world of neurodegenerative diseases, Alzheimer’s and related disorders known as tauopathies have long puzzled scientists. These conditions are characterized by the abnormal accumulation of tau protein in the brain, leading to the formation of toxic tangles that contribute to the progressive loss of brain cells. Despite decades of research, the precise mechanisms driving this pathological process have remained elusive, largely due to the lack of appropriate human models to study these diseases.
Now, a preclinical study, led by Weill Cornell Medicine researchers and published in the journal Cell, has developed a novel human stem cell-based model that faithfully recapitulates key features of tauopathies. By harnessing the power of induced pluripotent stem cells (iPSCs) and cutting-edge gene editing techniques, scientists engineered human neurons expressing a mutated form of tau protein, known as 4R-P301S, which is associated with a genetic form of frontotemporal dementia.
“Currently no therapies can stop the spread of tau aggregates in the brains of patients with Alzheimer’s disease,” says lead study author Dr. Li Gan, director of the Helen and Robert Appel Alzheimer’s Disease Research Institute and the Burton P. and Judith B. Resnick Distinguished Professor in Neurodegenerative Diseases in the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine, in a media release. “Our human neuron model of tau spread overcomes the limitations of previous models and has unveiled potential targets for drug development that were previously unknown.”
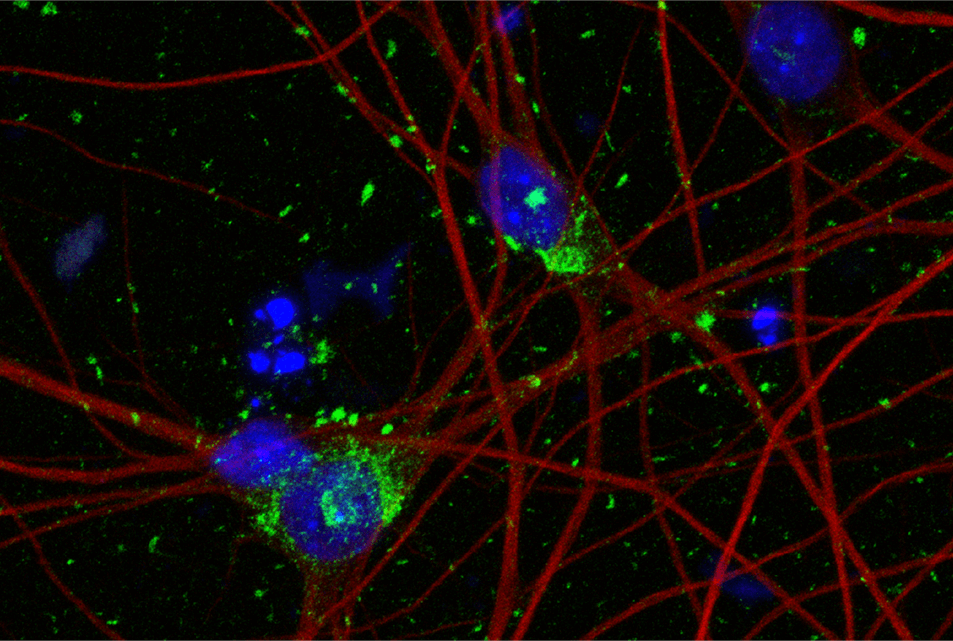
When exposed to tau fibrils, these 4R-P301S neurons exhibited progressive accumulation of tau tangles, mimicking the spreading of pathology observed in patient brains. The tau-bearing neurons also displayed abnormalities in cellular waste disposal systems, particularly in structures called endolysosomes, as well as reduced electrical activity. These findings suggest that the model captures not only the defining pathological hallmarks but also the functional impairments associated with tauopathies.
To identify the genetic factors influencing the propagation of tau pathology, the researchers performed a CRISPR interference (CRISPRi) screen, which allowed them to systematically inhibit the expression of over 1,000 genes suspected to play a role in tau biology. This unbiased approach led to the discovery of more than 500 genes that either promoted or suppressed the formation of tau aggregates when silenced. Among the top hits were genes involved in cellular trafficking pathways, such as VPS29, a component of the retromer complex that shuttles proteins between different compartments within the cell.
“CRISPRi technology allowed us to use unbiased approaches to look for drug targets, not confined to what was previously reported by other scientists,” explains study co-author Celeste Parra Bravo, a neuroscience doctoral candidate in the Weill Cornell Graduate School of Medical Sciences working in the Gan lab.
Researchers were intrigued when the screen also revealed a previously unrecognized role for the UFMylation cascade, a biological pathway that attaches a small protein called UFM1 to other proteins, in modulating tau aggregation. Inhibiting key enzymes in this cascade, such as UBA5 and UFM1 itself, significantly reduced the burden of tau inclusions in the human neuronal model. These findings were further validated in a mouse model of tau pathology, where blocking UBA5 expression in the brain attenuated the spreading of tau aggregates from one brain region to another.
The potential clinical relevance of these discoveries was underscored by the observation that the UFMylation pathway is altered in the brains of patients with progressive supranuclear palsy and Alzheimer’s disease. Specifically, neurons bearing neurofibrillary tangles exhibited reduced levels of free UFM1 protein compared to neighboring tangle-free neurons, suggesting that dysregulation of UFMylation may contribute to the pathogenesis of these disorders.
By shedding light on the complex cellular mechanisms underlying the formation and propagation of tau aggregates, this study opens up new avenues for the development of targeted therapies for tauopathies. The human stem cell-based model provides a robust platform for further dissecting the molecular pathways driving tau pathology and for screening potential therapeutic compounds. Moreover, the identification of the UFMylation cascade as a key regulator of tau aggregation offers a promising new target for intervention strategies aimed at slowing or halting the progression of these devastating diseases.

“We are particularly encouraged by the confirmation that inhibiting UFMylation blocked tau spread in both human neurons and mouse models,” concludes study co-author Dr. Shiaoching Gong, associate professor of research in neuroscience in the Appel Institute at Weill Cornell Medicine.
As our population ages and the burden of neurodegenerative disorders continues to grow, innovative approaches like this one offer renewed hope in the fight against Alzheimer’s and related tauopathies. By harnessing the power of stem cells, gene editing, and unbiased genetic screens, scientists are poised to unravel the mysteries of these complex diseases and develop effective treatments to improve the lives of millions affected by these conditions worldwide.












