Could a cure for the deadliest form of brain cancer finally be on the horizon? Researchers at the University of Florida have developed a personalized mRNA brain cancer vaccine that rapidly mobilized the immune system to attack glioblastoma. The results, published in the journal Cell, offer a glimmer of hope for patients facing this devastating diagnosis.
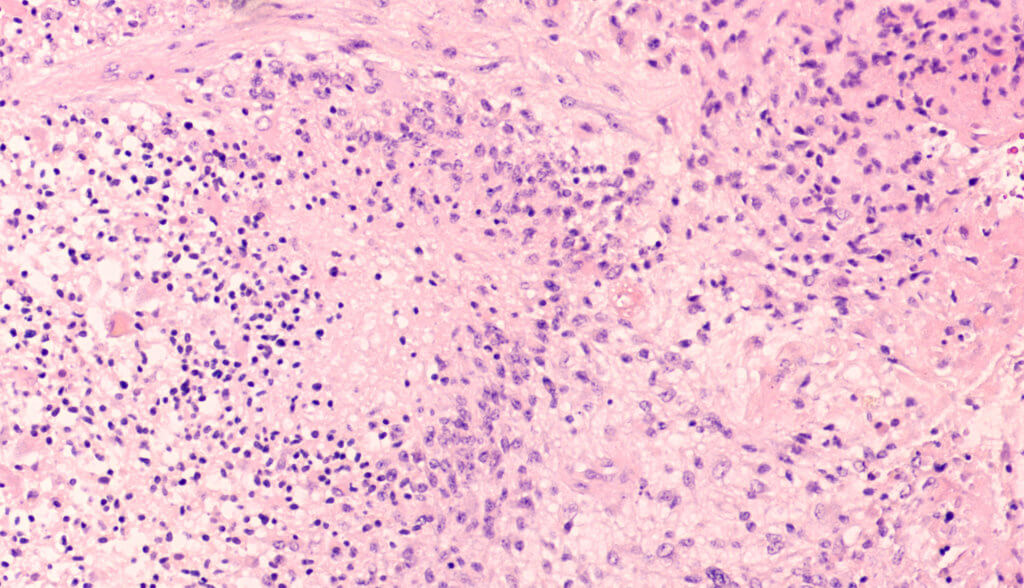
Glioblastoma is an incredibly aggressive brain tumor with a median survival of just 15 months. Current treatments involve surgery, radiation, and chemotherapy, but even with this multi-pronged approach, the prognosis remains grim. That’s why the findings from this first-in-human clinical trial are so exciting.
The new vaccine uses a similar mRNA technology to the COVID-19 vaccines that have become household names, but with a twist. Instead of delivering a pre-determined viral protein, the cancer vaccine is personalized using the patient’s own tumor cells. This allows the immune system to be trained to recognize and attack the specific mutations present in an individual’s cancer.
“Instead of us injecting single particles, we’re injecting clusters of particles that are wrapping around each other like onions, like a bag full of onions,” says senior study author Dr. Elias Sayour, a University of Florida Health pediatric oncologist who pioneered the new vaccine, in a media release. “And the reason we’ve done that in the context of cancer is these clusters alert the immune system in a much more profound way than single particles would.”
When the vaccine was delivered intravenously to four adult patients with glioblastoma, the results were striking. Within just 48 hours, the tumors shifted from “cold” — meaning they had very few immune cells and a silenced immune response — to “hot,” with a very active immune response.
“That was very surprising given how quick this happened, and what that told us is we were able to activate the early part of the immune system very rapidly against these cancers, and that’s critical to unlock the later effects of the immune response,” explains Dr. Sayour.
Before advancing to the human trial, the vaccine was tested in preclinical mouse models and a clinical trial of 10 pet dogs with spontaneously developed terminal brain cancer. Dogs are the only other species that naturally develops brain tumors with any frequency, making them a valuable model for studying gliomas, which are universally fatal in canines. The dogs in the trial, treated with their owners’ consent, lived a median of 139 days compared to the typical 30-60 day survival.
While it’s too early in the human trial to fully assess the clinical effects, the patients either lived disease-free or survived longer than expected. The next step is to expand the trial to include up to 24 adult and pediatric patients to validate the findings, and if an optimal and safe dose is confirmed, move on to a Phase 2 trial with an estimated 25 children.
“The demonstration that making an mRNA cancer vaccine in this fashion generates similar and strong responses across mice, pet dogs that have developed cancer spontaneously and human patients with brain cancer is a really important finding, because oftentimes we don’t know how well the preclinical studies in animals are going to translate into similar responses in patients,” notes study co-author Dr. Duane Mitchell, director of the University of Florida Clinical and Translational Science Institute and the Brain Tumor Immunotherapy Program. “And while mRNA vaccines and therapeutics are certainly a hot topic since the COVID pandemic, this is a novel and unique way of delivering the mRNA to generate these really significant and rapid immune responses that we’re seeing across animals and humans.”
Researchers are hopeful that this could represent a new paradigm for treating patients and a platform technology for modulating the immune system.
“I am hopeful for how this could now synergize with other immunotherapies and perhaps unlock those immunotherapies. We showed in this paper that you actually can have synergy with other types of immunotherapies, so maybe now we can have a combination approach of immunotherapy,” says Dr. Sayour.
While there is still uncertainty about how to best harness the immune system while minimizing side effects, these results represent a major step forward in the fight against one of the most lethal cancers. For patients and families facing a glioblastoma diagnosis, this personalized mRNA vaccine offers a beacon of hope on the horizon. With further research and clinical trials, it may one day transform the landscape of brain cancer treatment.












