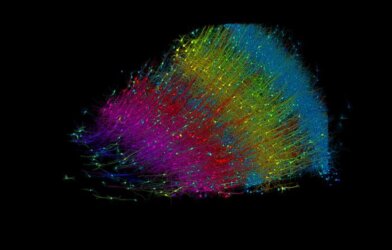
A revolutionary new treatment for Alzheimer’s disease could soon be on the way thanks to lab grown “mini-brains.” Scientists from the University of Saskatchewan have developed a method to grow miniature models of the human brain, known as brain organoids, that closely resemble the cellular composition and protein expression patterns of the actual human brain. This research, published in the journal Frontiers in Cellular Neuroscience, paves the way for more accurate studies of human brain health and disease using these lab-grown brain models.
Brain organoids are 3D structures grown from human stem cells that mimic the structure and function of the developing human brain. While they have been used in research for over 15 years, it was unclear how well they truly represented the human brain at the molecular level. The current study aimed to address this question by comparing the protein expression patterns in brain organoids to those found in human brain tissue samples.
“Never in our wildest dreams did we think that our crazy idea would work,” says lead study author Dr. Tyler Wenzel, a postdoctoral fellow in the College of Medicine’s Department of Psychiatry at the University of Saskatchewan. “These could be used as a diagnostic tool, built from blood.”
Canadian researchers first optimized the conditions for growing brain organoids, discovering that the initial 24 hours of the process are critical in determining the cell types and composition of the resulting organoids. By fine-tuning the nutrient balance during this period, they were able to consistently produce brain organoids containing all the major cell types found in the human brain, including neurons, astrocytes, oligodendrocytes, and microglia.
The team found that using stem cells derived from male and female siblings resulted in brain organoids with very similar growth rates, sizes, and protein content. This suggests that the genetic background of the stem cells plays a key role in the consistency of the organoids, and using related stem cell lines could help reduce variability in future studies.
“If stem cells have the capacity to become any cell in the human body, the question then came ‘could we create something that resembles an entire organ?’” notes Dr. Wenzel. “While we were developing it, I had the crazy idea that if these truly are human brains, if a patient had a disease like Alzheimer’s and we grew their ‘mini-brain,’ in theory that tiny brain would have Alzheimer’s.”
To assess how closely the brain organoids resembled actual human brain tissue, the researchers compared the protein expression patterns, or “protein banding patterns,” between the organoids, human brain samples from the cortex and cerebellum, and mouse brain samples. They found that the protein banding patterns in the brain organoids were much more similar to those in the human brain samples than to those in the mouse brain.
This finding is significant because it suggests that brain organoids are processing and expressing proteins in a human-specific manner, making them a more accurate model for studying human brain function and disorders. Many neurological and psychiatric conditions are thought to involve abnormalities in protein processing, such as alternative splicing and post-translational modifications. Having a human-specific model system that captures these processes could greatly advance our understanding and treatment of these conditions.
The study also found that brain organoids grown using their optimized method displayed neural network activity, as measured by electrical signals, as early as three months in culture. This is a much shorter timeframe than previously reported for other brain organoid protocols, some of which require up to six months to achieve similar levels of functional maturity. The presence of innate microglia, the immune cells of the brain, in these organoids may be contributing to this accelerated development.
“I’m still in disbelief, but it’s also extremely motivating that something like this happened,” concludes Dr. Wenzel. “It gives me something that I think will impact society and have actual relevance and create some change… it has a strong potential to shift the landscape of medicine.”