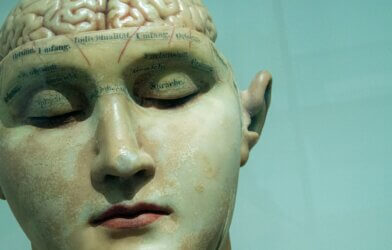
Neurostimulation devices are used to administer deep brain stimulation as a form of treatment for those with diseases such as Parkinson’s and epilepsy. Electrodes inactivate specific neural pathways causing activity in brain areas associated with these diseases to cease.
For several years, scientists have speculated that deep brain stimulation may be used to treat depression, specifically in patients who have not benefited from conventional therapies. However, because the regions of the brain affected by depression differ across individuals, it is necessary to modify existing technologies to make them better suited to treat depression.
Researchers from the University of California at San Francisco (UCSF) have now published a case report of a young woman by the name of Sarah who suffered from treatment-resistant severe clinical depression. Doctors were able to effectively treat her with a neurostimulation device tailored to her unique needs.
According to Dr. Katherine Scangos, assistant professor of psychiatry at the UCSF Weill Institute for Neurosciences and the paper’s main author, this discovery suggests that psychiatrists may be capable of providing more customized future treatments.
“Evidence this kind of therapy can work provides hope to patients and is certainly something that is meaningful to me, in that we as psychiatrists will be able to help people with mental illness,” said Dr. Scangos. “I think it suggests there could be a whole other type of treatments that are based on biomarkers that can deliver treatment in short time frames rather than antidepressants, which act on much longer time frames.”
Identifying a Biomarker for Depression
The researchers’ initial task was to identify a “biomarker” that would signal Sarah’s depression. This data would enable them to recognize the aberrant brain activity that is producing the depression, allowing them to focus the electrical pulses at the correct location and the most opportune time. Since current neurostimulation devices provide continual electrical pulses to the brain, researchers sought a means to identify and interrupt depression-related brain activity whenever it occurred.
To make this possible, the team used brain mapping which involved inserting ten electrodes over Sarah’s left and right hemispheres and monitoring cerebral activity for ten days. Throughout this period, Sarah used symptom rating measures to assess the intensity of her depression symptoms. The team discovered that gamma waves in the amygdala, an inner region of the brain, were most strongly linked to depressive symptoms, suggesting they could serve as a biomarker to indicate her depression.
The team then had to find a way to prevent these brain waves from happening. After identifying irregular activity throughout the amygdala, they administered electrical stimulation. This led to the discovery that inserting an electrode in the ventral capsule/ventral striatum near the brainstem produced the most continuous alleviation of symptoms.
The method was optimized, and it turned out that using extremely little quantities of electricity (1 milliampere or 1mA) for only 6 seconds each time was enough to relieve Sarah’s symptoms.
Curing Sarah
Sarah, who had suffered from major clinical depression from childhood, began the experiment with a Montgomery-Asberg Depression Rating Scale score of 36/54, which indicates the intensity of bouts of depression. Her depression had not improved with medicines or electroconvulsive treatment. However, she stated that after commencing therapy with the electrical stimulation device, her depression decreased from 33/54 to 14/54 within a span of only 12 days. It subsequently went below 10 within a few months of commencing therapy and has remained there for 15 months, indicating that she is no longer depressed.
On the one hand, this case report only shows the therapy’s success in one individual. However, the study provides a technique to modify this neurostimulation, demonstrating that this approach can be customized for the future treatment of psychiatric illnesses.
“Regarding the study in question, we are learning, especially in the fields of neurology and psychiatry, that many of the syndromes we treat are complex and heterogeneous, and we cannot expect that ‘one size treatment fits all.’ Patients with overlapping symptoms may have very different pathways for their development,” said Dr. Robert Greenberg, an associate clinical professor of psychiatry at the New York University School of Medicine. “This has led to recent attempts to understand the individual pathophysiology of disorders and individualize treatment to a much greater degree than previously possible.”
Since Sarah’s tests, the research team has recruited two additional participants in a study and intends to recruit nine more in the near future.
The details of the case study appear in the journal Nature Medicine.