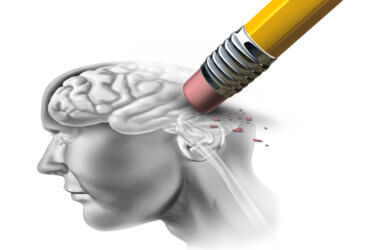
Removing the brain’s chemical messengers related to addiction and wakefulness may ease the symptoms of withdrawal from opioids and reduce risk of relapse. The potentially game-changing procedure was conducted on mice by scientists at UCLA.
The basis for the study stems from another UCLA study in 2000 that found human narcolepsy could be traced to a loss of approximately 90% of the 80,000 brain cells that contain hypocretin (also called orexin). Hypocretin is one of the brain’s chemical messengers significant in regulating sleep and wakefulness.
Patients diagnosed with narcolepsy are often treated with drugs that would be considered highly addictive for the average person. However, narcoleptic individuals on these medications have shown little to no indication of drug dependence, addiction, or withdrawal symptoms.
The substantial loss of hypocretin-producing neurons and lack of drug addiction experienced by narcolepsy patients again became of interest when researchers later discovered that people with a heroin addiction have an average of 54% more hypocretin-producing neurons than non-addicts. They tested mice and found the same pattern of heightened hypocretin, lasting as long as four weeks after stopping opioid treatments.
Researchers believe that their study may have identified a notable cause of drug cravings, while also bringing added understanding to why narcoleptics do not typically experience addiction. Future research will continue to confirm and expand upon these findings. Signs indicate that the development of medications targeting the hypocretin system may produce favorable results in the treatment of addiction.
In their most recent study, researchers at UCLA raised the amount of hypocretin-producing neurons in a group of mice. Results show that mice treated with opioids responded with an increase in hypocretin levels in the area of the brain that regulates symptoms of withdrawal, called the locus coeruleus (LC).
These higher levels of hypocretin in the LC also increased the level of tyrosine hydroxylase (TH) enzymes present in the body, which sparks norepinephrine (NE) production. These neurons in the LC create more NE and distribute it throughout the brain, using it to stimulate arousal, wakefulness, attention, or a “fight or flight” stress response.
A commonly theorized cause of opioid withdrawal symptoms stems from the neurological response to stopping the drug. When an addicted individual stops taking opioids, the LC activity spikes, triggering the production and release of more NE, which many scientists believe plays a significant part in withdrawal.
Researchers expected to see a reduction in withdrawal symptoms after removing hypocretin-producing neurons. Their hypothesis was confirmed when their findings showed the removal of hypocretin-producing neurons resulted in the reduction of both physical and emotional symptoms associated with opioid withdrawal and halted rising levels of TH in the LC.
Further research will be required, but the findings of this study suggest that drug treatments targeted at the hypocretin system could have positive effects on patients suffering from opioid addiction.
This study is published in the Journal of Neuroscience.
Report written by Anna Landry