Is a cure for blindness on the horizon? In a pioneering study published in the journal Advanced Healthcare Materials, an international research team has demonstrated the potential of highly flexible, polymer-based brain implants for restoring vision over extended periods. These innovative devices could pave the way for more effective and durable visual prosthetics in the future.
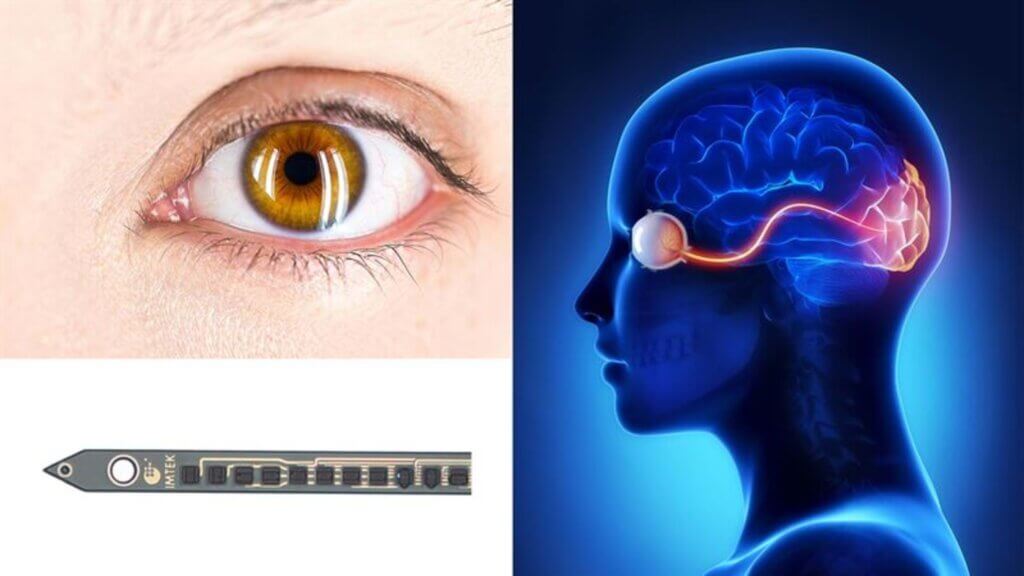
The field of neuroprosthetics has made significant strides in recent years, with numerous studies showing that electrical stimulation of the brain via implanted electrodes can generate complex sensory experiences. In the realm of vision, stimulating neurons in the visual cortex can elicit the perception of light spots known as “phosphenes.”
However, a major challenge in creating clinically viable visual prosthetics has been the degradation of implant functionality over time. Conventional silicon-based electrode arrays, such as the Utah array, often suffer from deteriorating performance due to factors like material instability, electrode degradation, and the brain’s foreign body response.
To overcome these obstacles, researchers from Chalmers University of Technology in Sweden, University of Freiburg and the Netherlands Institute for Neuroscience turned to ultra-flexible, polymer-based electrode arrays. These devices are made of thin polyimide shanks, measuring a mere 10 micrometers in thickness, and feature several small electrodes, each smaller than 15 micrometers.
The flexibility of these polymer probes allows them to move with the brain tissue during natural movements like respiration and heartbeat, minimizing damage and inflammation. Additionally, their small size ensures minimal disruption of blood flow within the brain.
“This image would not be the world as someone with full vision would be able to see it. The image created by electrical impulses would be like the matrix board on a highway, a dark space and some spots that would light up depending on the information you are given. The more electrodes that ‘feed’ into it, the better the image would be,” says study co-author Maria Asplund, who led the technology development part of the project and is professor of Bioelectronics at Chalmers University of Technology.
In a series of in vitro tests, researchers demonstrated the remarkable stability of these polymer electrodes. Even after applying billions of electrical pulses, mimicking years of continuous use, the electrodes showed little to no degradation in performance.
To evaluate the real-world effectiveness of these devices, the team implanted the flexible arrays into the primary visual cortex (V1) of mice. The animals were then trained to detect and report the perception of phosphenes triggered by electrical microstimulation.
The mice were able to consistently detect stimulation at current levels as low as 2-20 microamperes, which is well below the maximum currents the electrodes can safely deliver. This suggests that the reduced foreign body response elicited by the flexible implants allows for effective neuronal activation at lower stimulation thresholds.
“Miniaturization of vision implant components is essential. Especially the electrodes, as they need to be small enough to be able to resolve stimulation to large numbers of spots in the ‘brain visual areas,'” explains Asplund. “The main research question for the team was, ‘can we fit that many electrodes on an implant with the materials we have and make it small enough and also effective?’ and the answer from this study was — yes.”
Perhaps most impressively, the functionality of these polymer-based devices remained stable for up to a year after implantation — a substantial improvement over the typical lifespan of silicon-based arrays. Histological analysis of the brain tissue surrounding the implants revealed only limited signs of inflammation and glial scarring, further evidencing the biocompatibility of the flexible probes.
While this study was conducted in mice, the implications for human visual prosthetics are significant. If these results can be replicated in larger animals and eventually in human trials, it could mean a major leap forward in the development of long-lasting, high-resolution visual prosthetics.
The ability to restore sight to the blind or visually impaired would be life-changing for millions worldwide. Beyond the immediate benefits to quality of life, such technology could also open up new opportunities for education, employment, and social engagement.
“The conducting polymer metal combination we have implemented is revolutionary for vision implants as it would mean they hopefully could remain functional for the entire implant life-time,” notes Asplund. “We now know it is possible to make electrodes as small as a neuron (nerve cell) and keep this electrode effectively working in the brain over very long timespans, which is promising since this has been missing until now. The next step will be to create an implant that can have connections for thousands of electrodes.”
There is still much work to be done before these flexible polymer implants can be translated into clinical devices. Further research will be needed to optimize the implantation process, develop wireless power and data transmission systems, and ensure the long-term safety and efficacy of the technology.












