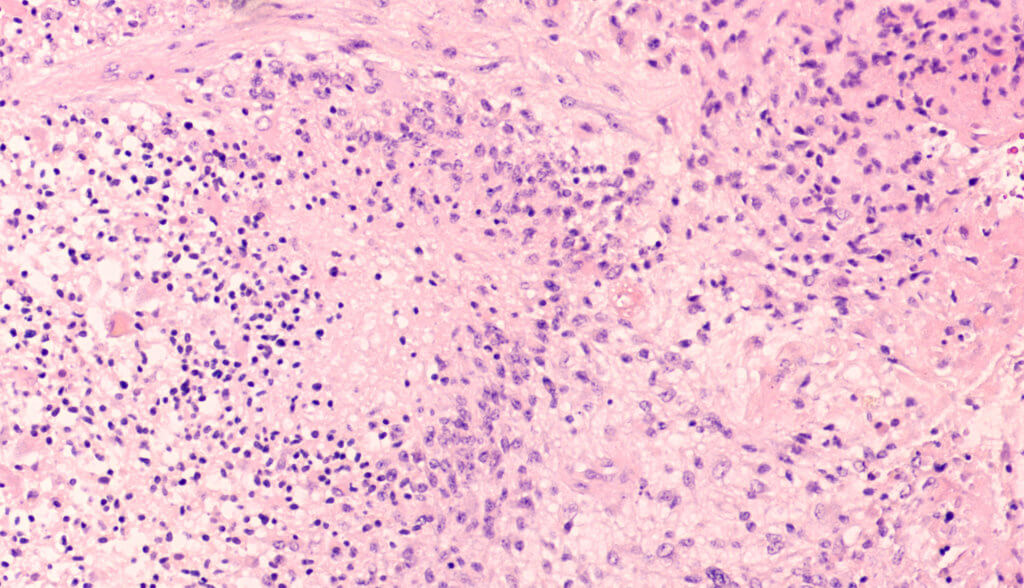
Glioblastoma is one of the most common and deadly brain cancers. It is an aggressive cancer that can occur in the brain or spinal cord. Glioblastoma forms from astrocytes – cells that support nerve cells. It can affect anyone. Only 5% of patients survive more than 5 years from diagnosis. It presents with worsening headaches, nausea, vomiting, and seizures. Glioblastoma, also known as glioblastoma multiforme, can be very difficult to treat and a cure is often not possible. Treatments may only slow progression of the cancer and reduce signs and symptoms.
The Biden family has been plagued by assaults on the brain. In 1972, President Joe Biden’s first wife, Neilia Hunter Biden, with her one-year-old daughter Naomi, died in a car crash. Their two sons, Beau, age 4, and Hunter, age 3, were both critically injured. Hunter sustained a skull fracture and severe traumatic brain injuries. In 1988, Joe underwent emergency surgery for two potentially deadly intracranial aneurysms. In 2010, Beau suffered a stroke, then died of brain cancer in 2015. The family chose not to disclose the type of brain cancer. A glioblastoma is one possibility.
“A major therapeutic challenge is the variability and adaptability of these brain tumor cells. From patient to patient, glioblastoma tumors are composed of several types of cells in varying proportions. It’s these variations and their incredible capacity to quickly change their identity to hide and escape treatments that make them challenging to eradicate,” says co-author Cedric Bardy from Flinders University, South Australia, and South Australian Health and Medical Research Institute (SAHMRI), in a statement.
Bardy’s team is hopeful of finding a new method to treat the deadly disease. “Recent advances in genetics have shown that the cell types found within glioblastomas resemble their cells of origin, before they became cancerous. They also use molecular pathways common with healthy brain cells for growth, survival or changing their identity,” says Bardy, in a statement
“What our research suggests is that we may learn from the genetics of healthy brain cells in order to target vulnerabilities in glioblastoma cancer cells,” says Inushi De Silva, a PhD student with Flinders University and SAHMRI.
“Brain cells are not as good as cancer cells in being able to quickly change their identity in response to environmental changes, so if we manage to exploit and amplify this hidden inherited genetic weakness in cancer cells, we might be able to reverse their ability to escape treatments,” De Silva explains.
“We should be able to use this in targeted therapy, with treatments that restrict glioblastoma tumor cells ability to change, a quality known as plasticity. Understanding more about these mechanisms will be helpful to develop new treatments in the future,” says Bardy.
“Glioblastoma cells are tough to kill because they are such a fast-moving target. This review helps us understand the different pathways in which they can hide. If we can block them in a corner, we may have a better chance to hit the target and cure this terrible disease,” Bardy concludes.
The study is published in the journal Trends in Cancer.