Taking Prozac Immediately After Trauma May Prevent Mental Damage, Mouse Study Suggests
Fear is a natural survival mechanism that keeps us alert and safe from danger. But for those who have experienced severe or life-threatening stress, fear can become a constant companion, even in the absence of tangible threats. This generalized fear can be psychologically damaging and lead to debilitating conditions like post-traumatic stress disorder (PTSD). Now, a team of neurobiologists at the University of California San Diego are sharing a major discovery that sheds light on the brain chemistry and neural circuitry behind this phenomenon, opening new avenues for prevention and treatment.
In a study published in the journal Science former UCSD Assistant Project Scientist Hui-quan Li (now a senior scientist at Neurocrine Biosciences), Atkinson Family Distinguished Professor Nick Spitzer, and their colleagues have identified a surprising mechanism at the root of stress-induced generalized fear: a switch in the chemical messengers, or neurotransmitters, that allow brain cells to communicate with each other.
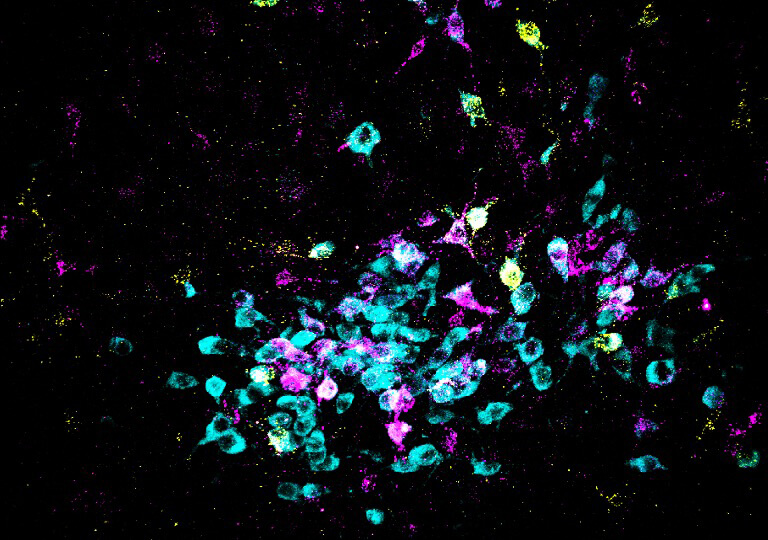
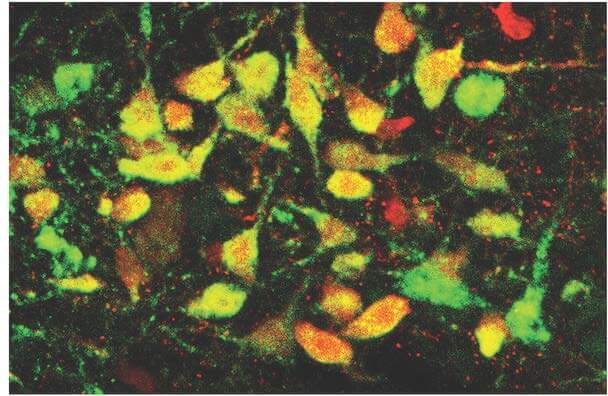
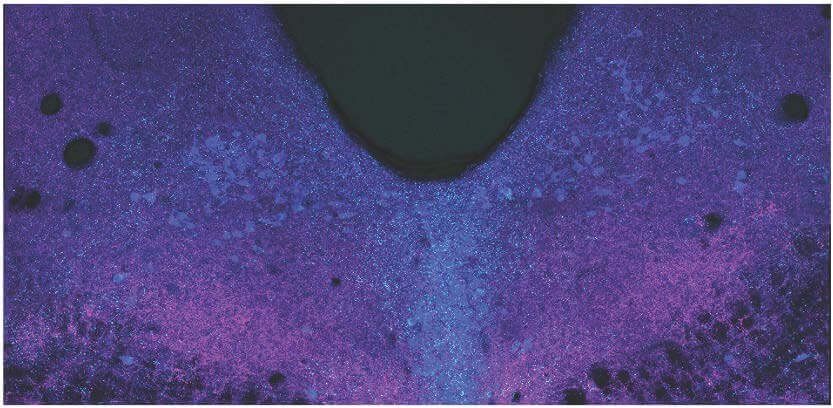
The researchers focused on a brain region called the dorsal raphe, located in the brainstem. They found that when mice experienced an intensely stressful event (in this case, a series of strong electric foot shocks), the neurons in this area underwent a dramatic changeover. The cells began producing less glutamate, a neurotransmitter that tends to activate other neurons, and more GABA, which tends to quiet them down. This “transmitter switch” emerged within three days of the stressful event and persisted for at least a month.
Intriguingly, the neuronal language swap seemed to go hand-in-hand with a striking behavioral change. Mice that had undergone the switch began freezing in fear not just in the chamber where they’d been shocked, but in completely new environments that should have felt safe—a clear sign of generalized fear.
To confirm the link between the transmitter switch and generalized fear, the researchers used cutting-edge genetic techniques to prevent the switch from occurring in stressed mice. Remarkably, this intervention stopped the mice from developing generalized fear, suggesting that the switch is a critical step in the process. The team also examined postmortem brain tissue from humans with PTSD and found evidence of the same kind of neurotransmitter shift seen in the mice, hinting at a similar mechanism in clinical anxiety.
“Our results provide important insights into the mechanisms involved in fear generalization,” said Spitzer, a member of UC San Diego’s Department of Neurobiology and Kavli Institute for Brain and Mind, in a statement. “The benefit of understanding these processes at this level of molecular detail—what is going on and where it’s going on—allows an intervention that is specific to the mechanism that drives related disorders.”
Further investigation revealed that the transmitter switch is triggered by a complex cascade of hormonal signals that kick into gear when the brain senses danger. The researchers found they could mimic the effects of foot shocks by artificially boosting the mice’s levels of cortisol, a key stress hormone, or by stimulating the brain cells that secrete a related hormone called CRH. Conversely, they could block the switch—and the development of generalized fear—by interfering with CRH-secreting neurons or the receptor for cortisol.
Perhaps most excitingly, the team discovered that a common antidepressant medication, fluoxetine (better known as Prozac), could prevent both the neurotransmitter changeover and the emergence of pervasive fear when given to mice immediately after the foot shocks. However, if the drug was administered after the switch had already occurred, it was much less effective—a finding that aligns with clinical observations that PTSD becomes increasingly difficult to treat over time.
In addition to pinpointing the location of the “fear-switching” neurons, the researchers mapped their connections to the central amygdala and lateral hypothalamus, brain regions previously linked to other fear responses. “Now that we have a handle on the core of the mechanism by which stress-induced fear happens and the circuitry that implements this fear, interventions can be targeted and specific,” said Spitzer.
While more research is needed to translate these findings to humans, the implications are profound. By shedding light on the biological underpinnings of paralyzing anxiety, the study points toward new strategies for preventing PTSD in recently traumatized individuals and improving treatments for those already struggling with the disorder. It also underscores the brain’s remarkable capacity to rewire itself in response to harrowing experiences—for better or worse.
As we continue to unravel the complex languages of the brain, studies like this bring us closer to finding ways to quiet the voices of fear when they threaten to drown out everything else. With targeted interventions on the horizon, there is renewed hope for those living in the shadow of trauma.