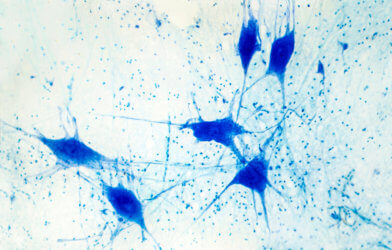
The treatment of most neurological disorders, such as Alzheimer’s and Parkinson’s diseases, requires infiltration of the brain’s natural barrier, called the blood-brain barrier. This protective layer is made of specialized cells called astroglia that span the entire surface of the central nervous system. Their main function is to prevent toxins from entering the neurons of the brain while enabling cells to receive nutrients from the blood. However, these cells detect beneficial medications as toxins, forming a roadblock for this method of treatment.
According to scientists, the only way in which to deliver effective doses of medicine is to supply the brain with extremely large amounts of a drug at a time. This technique, however, only delivers tiny portions of the drug to brain cells, rendering it ineffective, and dangerous in terms of severe adverse effects.
With the help of Professor Charles Ramassamy or the Institut National de la Recherche Scientifique (INRS), Jean-Michel Rabanel, a postdoctoral researcher, is working to find a way to bypass the barrier with nanoparticles covered in a special polymer. According to the latest research, having a polymerized substance enhances the overall receptivity of the drug to the astroglial cells, enabling the crossing of the nanoparticles through the blood-brain barrier.
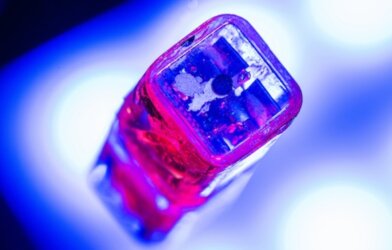
For the research, Rabanel chose two types of substances to test. The first consisted of polyethylene glycol (PEG) which had previously shown positive results in the translucent bodies of zebrafish. The second consisted of a neutrally charged “zwitterionic” substance that more closely imitated proteins commonly found in cell membranes. The team tested both polymer coverings on the nanoparticles which are made of polylactic acid (PLA), a non-toxic substance that is quickly eliminated as waste.
“With this type of experiment, we demonstrated that the zwitterionic polymer, which in theory is more biocompatible since it’s similar to molecules at the cell’s surface, have a better access to the brain. However, it is more rapidly absorbed by blood vessel walls, which reduces their circulation time,” explains Ramassamy in a release.
In other words, results indicated that although the neutral substance proved more successful at infiltrating the blood-brain barrier, it is disposed of quicker, making it less potent than PEG. According to Professor Ramassamy, combining the two substances into one polymer coating may be the best method to treat these neurological diseases.
“Our findings demonstrate that the drug coating is a very important factor in the therapeutic use of nanoparticles. It’s an interesting avenue for delivering drugs directly to the brain and improving the treatment for neurodegenerative diseases,” said Ramassamy, who also holds the Louise and André Charron Research Chair on Alzheimer’s Disease at the Armand-Frappier Foundation.
Currently, there are approximately 6.2 million Alzheimer’s patients in the United States, according to the Alzheimer’s Disease Association (ADA). Considering all types of neurological disorders worldwide, this number is closer to 1 billion.
This research is published in Biomaterials.










Comments