There’s new hope for older adults struggling with depression and anxiety. A new study from the University of Florida suggests that a non-invasive brain stimulation technique called transcranial direct current stimulation (tDCS) could help alleviate their symptoms. The findings, published in the journal Brain Stimulation, offer hope for a safe and effective alternative to medication for managing mental health in later life.
University scientists analyzed data from the Augmenting Cognitive Training in Older Adults (ACT) trial, which involved 378 participants aged 65-89. Participants received either active tDCS or a sham treatment while completing computerized cognitive training exercises over a 12-week period.
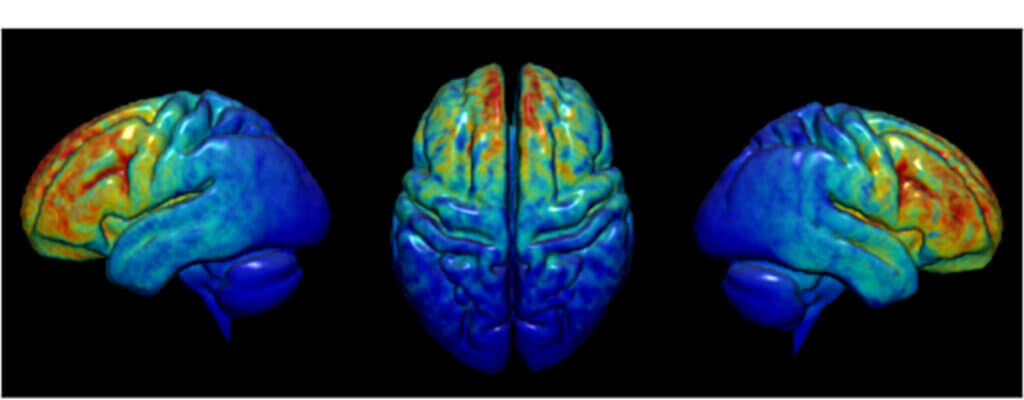
What exactly is tDCS? It involves applying a weak electrical current to specific areas of the brain through electrodes placed on the scalp. The current is thought to modulate the activity of brain regions involved in mood regulation, such as the dorsolateral prefrontal cortex (dlPFC). While tDCS has shown promise in treating clinical depression, its effects on milder, subclinical symptoms in older adults have been less well studied.
The ACT trial participants were not diagnosed with psychiatric disorders but did report varying levels of depression and anxiety symptoms at the start of the study. Researchers used standardized questionnaires to assess changes in these symptoms immediately after the intervention and again at a one-year follow-up.
The results were encouraging. Compared to the sham group, participants who received active tDCS showed greater reductions in both depression and state anxiety (temporary anxiety related to a specific situation) after the 12-week intervention. These benefits were particularly pronounced for those who started with mild depression or moderate to severe state anxiety.
“Depression and anxiety can impact our overall mental health, cognitive function and ability to function independently as we age,” says study senior author Dr. Adam Woods, the associate dean for research and a professor of clinical and health psychology at the university’s College of Public Health and Health Professions and co-director of the university’s Center for Cognitive Aging and Memory Clinical Translational Research, in a media release. “Often, front-line treatments involve medication and/or therapy, which can both be effective. However, there is also a pressing need for accessible and noninvasive options that can be deployed in people who are either nonresponsive to pharmaceutical treatment, unable to access or participate in clinic-based intensive treatment programs, or for a variety of other reasons.”
The anxiety-reducing effects of tDCS seemed to persist over time. Participants with moderate to severe state anxiety at baseline maintained their symptom improvements at the one-year mark if they had received active stimulation. This suggests that tDCS could have long-lasting benefits for some individuals.
It’s important to note that tDCS did not significantly impact trait anxiety, which refers to a more general tendency to feel anxious. Researchers speculate that this type of anxiety may be less amenable to short-term interventions like tDCS and may require longer-term treatments such as psychotherapy.
The study also found that certain demographic factors, such as age, sex, and education level, influenced mental health outcomes regardless of tDCS status. For example, women and older participants tended to report greater increases in depression and anxiety symptoms over time, while those with higher education levels showed greater symptom reductions. These findings highlight the need for personalized approaches to mental health treatment that take individual characteristics into account.
How does tDCS compare to other treatments for depression and anxiety in older adults? The most common approaches are medication and psychotherapy, but these can have drawbacks. Antidepressants and anti-anxiety drugs often come with side effects that can be particularly problematic for older individuals. Access to psychotherapy may be limited, and some people may not feel comfortable with talk therapy.
tDCS, on the other hand, is non-invasive, has minimal side effects, and can be administered in a relatively short timeframe. It also has the potential to be combined with other interventions, such as cognitive training, to enhance its benefits. While more research is needed to fully understand its mechanisms and optimize treatment protocols, tDCS represents a promising tool in the mental health toolkit for older adults.
“tDCS treatment is cost-effective, portable and can be seamlessly integrated with existing mental health therapies or used as a standalone intervention,” explains lead study author Hanna Hausman, clinical psychology doctoral student in neuropsychology. “Its potential for at-home self-administration would further expand accessibility and reduce personnel costs, making it a promising intervention for individuals who may experience barriers accessing face-to-face clinical care.”
This study has some limitations. The sample was predominantly white and non-Hispanic, so the findings may not generalize to more diverse populations. The study also did not directly compare tDCS to other treatments or look at its effects on diagnosed psychiatric disorders. Future research should address these questions to get a fuller picture of tDCS’s potential.
Researchers believe their findings offer hope that tDCS could be a safe and effective way to help older adults manage subclinical depression and anxiety symptoms. By targeting the brain directly, tDCS may provide relief for those who don’t respond well to or can’t access other treatments.