A non-invasive form of brain stimulation called repetitive transcranial magnetic stimulation (rTMS) was officially approved for depression treatment in 2008 by the U.S. Food and Drug Administration. Originally, it was offered to patients who didn’t originally respond well to antidepressants. Since then, it’s become more widespread, with other nations approving and recommending its use.
Previously, rTMS has shown promising improvements in up to half of patients who have resorted to this when standard treatments didn’t work. Given this, some researchers have thought that this would be a great technology to explore in older adults. Many of them suffer from different conditions, and taking several medications may dissuade them from adding antidepressants to the mix. However, since the early 2000s, many researchers have responded to this in disagreement, suggesting that it wouldn’t be beneficial at all.
Gonçalo Cotovio, a doctoral student in the Neuropsychiatry Unit, psychiatry resident in Centro Hospitalar de Lisboa Ocidental, and first author of a new paper on this topic, challenges this notion along with colleagues from Harvard Medical School and Iowa University. He says that previous studies based results off observing improvements after just 2 weeks of use, when currently approved rTMS treatments need 4-6 weeks to kick in.
Now, the team has put it to the test. Collaborating with other rTMS centres, 500 samples from those who received rTMS treatments to treat depression were collected, making this one of the largest sample sizes for this topic.
Patients were divided into two groups: one under 65, the other 65 or above. The results attained when comparing these two groups supported the teams’ doubts. Older adults responded just as well as the younger ones, but it took a bit longer to notice.
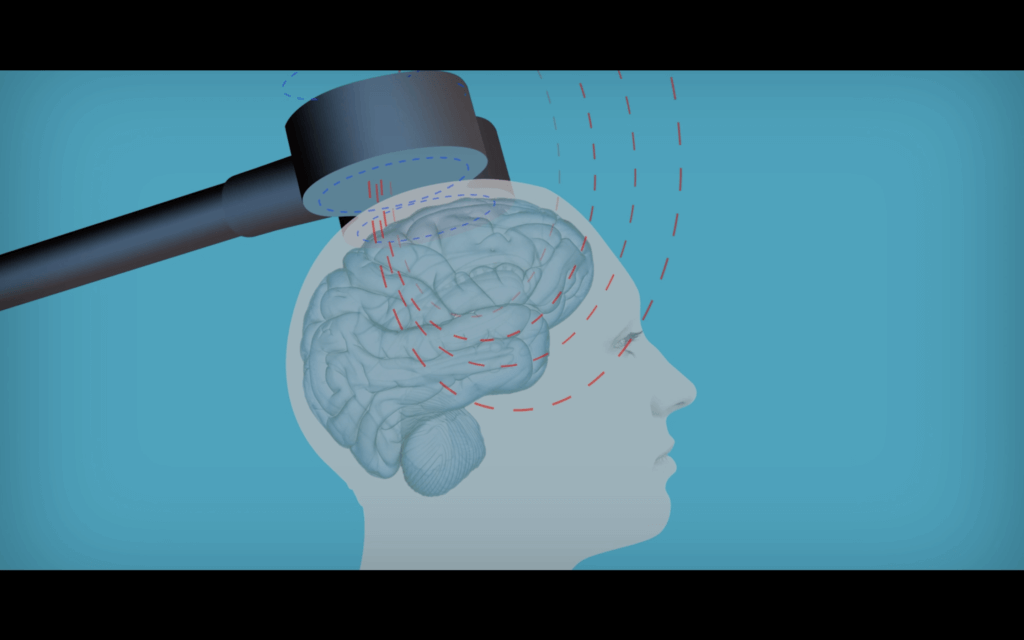
“Over the first two weeks of treatment, as the older data suggested, it is true that older patients showed little or no response to rTMS,” explains Gonçalo, “but the older group soon caught up and, by the end of the course of treatment, we observed that rTMS was just as effective as for younger patients.”
The researchers firmly believe that their work suggests that a full reconsideration of current policies and protocols put in place regarding rTMS use in older adults is crucial. Further studies could reinforce their findings, and help improve current treatment plan frameworks to be shifted to consider the longer amount of time it may take for elderly patients to see results.
“Hopefully this study may highlight the utility of rTMS as an important tool in treating depression for people of all ages,” concludes Gonçalo.
The study is published in the journal Frontiers in Aging Neuroscience.