There’s new hope in the fight against glioblastomas (GBMs) — the most aggressive and lethal type of brain tumor. These fast-growing tumors are notoriously difficult to treat, with patients typically surviving only about 15 months after diagnosis despite surgery, radiation, and chemotherapy. But now, a team of researchers at the University of Cincinnati Cancer Center is working to change that grim prognosis, thanks to a breast cancer drug.
The multidisciplinary team has launched a Phase 2 clinical trial to test a promising new treatment combination for recurrent GBMs. The trial is funded in part by a Catalyst Research Award from the Dr. Ralph and Marian Falk Medical Research Trust and the study is published in the journal Clinical Cancer Research.
So what makes glioblastomas so challenging to treat? Part of the problem is that they’re tough to catch early. These tumors often don’t cause noticeable symptoms until they’ve already grown quite large. Even after surgery to remove as much of the tumor as possible, GBMs frequently come back or develop resistance to follow-up radiation and drug treatments.
To make matters worse, many potential drug therapies can’t even reach the tumor cells because of the blood-brain barrier. This biological security system is great at protecting our brains from harmful toxins, but it only allows certain substances to pass from the bloodstream into the brain.
The Cincinnati team’s approach revolves around a drug called letrozole, which has been used to treat breast cancer for over two decades. Letrozole works by blocking an enzyme called aromatase that helps breast tumor cells grow. Crucially, the lab discovered that aromatase is also present in brain tumor cells, suggesting letrozole could work against glioblastomas too.
To put that idea to the test, researchers previously conducted a Phase 0/1 clinical trial of letrozole in glioblastoma patients. The results were encouraging.
“Letrozole was safe up to the highest dose, and there were no safety concerns in the Phase 0/1 trial,” says study author Dr. Trisha Wise-Draper, section head of Medical Oncology and professor in the Division of Hematology/Oncology in the University of Cincinnati’s College of Medicine, in a media release. “The biggest conclusion is that it was safe and that we could reach what we felt was going to be the effective dose based on Dr. Desai’s preclinical work.”
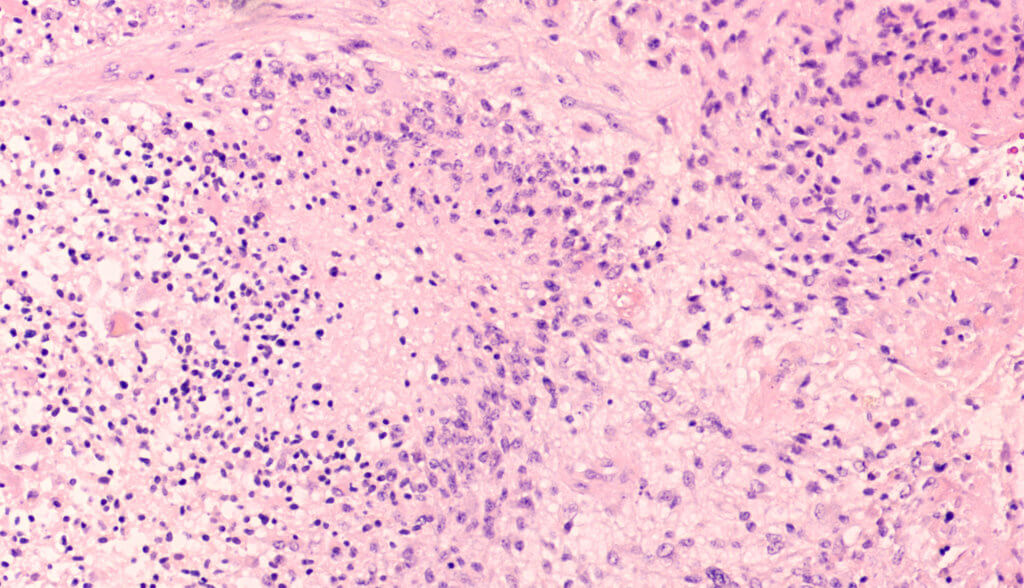
Importantly, when the team analyzed tumor tissue samples from patients, they found that letrozole was indeed crossing the blood-brain barrier to reach the cancer cells.
“We can categorically show that in humans the drug actually crosses and reaches the brain tumor at concentrations that we believe are likely to be most efficacious,” explains study author Dr. Pankaj Desai, professor and chair of the Pharmaceutical Sciences Division and director of the drug development graduate program in the University of Cincinatti’s James L. Winkle College of Pharmacy.
For the new Phase 2 trial, researchers are upping the ante by giving patients a combination of letrozole and the chemotherapy drug temozolomide, which is already approved for GBM. Dr. Desai said their preclinical research suggests this one-two punch could work better than letrozole alone. The trial will initially enroll 19 patients whose GBMs have come back after prior treatment and aren’t eligible for more surgery.
Looking ahead, the Cincinnati team is also collaborating to identify other drugs that could be paired with letrozole to battle glioblastomas even more effectively, supported by a $1.19 million grant from the National Institutes of Health.
“I think collaboration with multidisciplinary teams is critical to be able to have the expertise and all the components you need, including biostatistics, pharmacokinetics, clinical, basic science and neuro-oncology expertise,” notes Dr. Wise-Draper. “The future of all science is team science. No one really can do everything on their own anymore because we’re all too specialized.”

Dr. Desai emphasized the long road it’s taken to get to this point and the persistence required to translate research findings into real-world treatments.
“Only academic centers with integrated scientific and clinical expertise are able to move their molecules from the research bench to clinical trials,” says Dr. Desai. “It takes a lot of persistence, ups and downs, highs and lows of funding, but we have been supported by a very strong team of people. It’s a journey that has taken a while and a lot of hard work by a number of people, and we’re in a very exciting stage.”
With any luck, that exciting stage could lead to a brighter outlook for glioblastoma patients and their families. While much more research lies ahead, the Cincinnati team’s innovative efforts offer a glimmer of hope in the battle against this devastating disease.