A high-tech scanner that detects light deep inside the brain has been developed. It could boost cancer treatments and AI (artificial intelligence) and even lead to a screening program for Alzheimer’s disease.
The optical approach uses MRI (magnetic resonance imaging) to map how light spreads in opaque environments capturing dynamic changes in colors of tissue. It could map neuron-stimulating fibers during experiments or monitor patients receiving light-based therapies for tumors.
“We can image the distribution of light in tissue, and that’s important because people who use light to stimulate tissue or to measure from tissue often don’t quite know where the light is going, where they’re stimulating, or where the light is coming from. Our tool can be used to address those unknowns,” says senior author Alan Jasanoff, a professor of biological engineering, brain and cognitive sciences, as well as nuclear science and engineering, at MIT, in a statement.
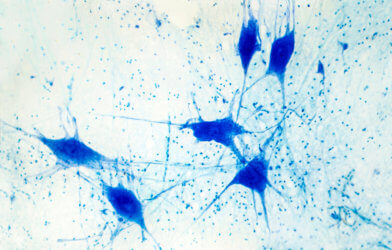
Light microscopes have been peering inside living cells and thin slices of tissue since the late 1500s, but can’t reach further.
“One of the persistent problems in using light, especially in the life sciences, is it doesn’t do a very good job penetrating many materials,” explains Jasanoff. “Biological materials absorb light and scatter light, and the combination of those things prevents us from using most types of optical imaging for anything that involves focusing in deep tissue.”
So his students helped design a sensor that could transform light into a magnetic signal.
“We wanted to create a magnetic sensor that responds to light locally, and therefore is not subject to absorbance or scattering. Then this light detector can be imaged using MRI,” says Jasanoff.
The lab has previously developed MRI probes that can interact with a variety of molecules in the brain, including the “feel-good” chemical dopamine and calcium.
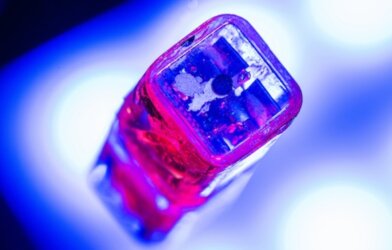
When they bind to their targets, it affects magnetic interactions with the surrounding tissue, dimming or brightening the signal. The light-sensitive version encases magnetic particles in a tiny bubbles of fat called liposomes. They become “leaky” when exposed to certain wavelengths.
The magnetic particles called liposomal nanoparticle reporters (LisNR) interact with water and generate a signal detectable by MRI. Researchers created particles that became leaky when exposed to ultraviolet light, and impermeable in blue light. There were also responses to other wavelengths.
Experiments on rats targeted a part of the brain called the striatum, which is involved in planning movement and responding to reward. After injecting the particles the researchers were able to map the distribution of light from an optical fiber implanted nearby.
It is similar to those used for optogenetic stimulation. So this kind of sensing could be useful to researchers who perform optogenetic experiments in the brain.
“We don’t expect that everybody doing optogenetics will use this for every experiment,” notes Jasanoff. “It’s more something you would do once in a while to see whether a paradigm you’re using is really producing the profile of light you think it should.”
The device could also be useful for monitoring patients receiving treatments that involve light. Photodynamic therapy, for instance, uses light from a laser or LED to kill cancer cells.
“This paper shows a novel sensor to enable photon detection with MRI through the brain,” says Dr. Xin Yu, of Harvard Medical School, who was not involved in the study. “This illuminating work introduces a new avenue to bridge photon and proton-driven neuroimaging studies.”
The researchers are now working on similar probes that could be used to detect light emitted by luciferases, or glowing proteins used in biological tests. It could reveal whether a particular gene is activated or not. Currently they can only be imaged in superficial tissue or cells grown in a lab dish.
Prof Jasanoff also hopes to use the strategy to design MRI probes that can detect stimuli other than light, such as neurochemicals or other molecules found in the brain.
“The principle we use to construct these sensors is quite broad and can be used for other purposes too,” says Jasanoff.
The study is published in Nature Biomedical Engineering.
Report by Mark Waghorn, South West News Service